What Can You Do to Improve Your Odds Against Cancer?
May 28, 2015 1 Comment
I sometimes joke with my patients that a new diagnosis of cancer rarely provides them enough time to get an MD or PhD. Yet it is that level of preparation that may be required to answer the myriad questions that lie ahead.
Although it’s a joke, it is only partly in jest. Unlike buying a house or a car for which one’s life experiences can prepare you, medicine is opaque, complicated and ever changing. At the bleeding edge of medical complexity sits medical oncology and its dizzying array of genomics, transcriptomics, proteomics, epigenomics and metabolomics. Not only is it difficult for patients to keep up with all the changes, it is increasingly beyond the ken of their doctors who have spent entire careers training in the specialty, many of whom may have an MD and a PhD.
So how can patients improve their odds when the obstacles seem so daunting?
 My first recommendation is that you develop a personal diary or record book of the procedures, staging studies, pathologic diagnosis, tumor markers, and physician recommendations. This can be accomplished by requesting that your doctors provide either electronic or physical copies of CT scans, pathology reports, blood tests and other clinically relevant information. While there has been some controversy surrounding their overuse, I am a believer in the simple blood tests used as barometers of your cancer with names like CEA, CA19.9, CA125, CA27.29, and CA 15.3. Although they are not perfect, they are easy to obtain, relatively inexpensive and can be repeated regularly to assess progress with therapy.
My first recommendation is that you develop a personal diary or record book of the procedures, staging studies, pathologic diagnosis, tumor markers, and physician recommendations. This can be accomplished by requesting that your doctors provide either electronic or physical copies of CT scans, pathology reports, blood tests and other clinically relevant information. While there has been some controversy surrounding their overuse, I am a believer in the simple blood tests used as barometers of your cancer with names like CEA, CA19.9, CA125, CA27.29, and CA 15.3. Although they are not perfect, they are easy to obtain, relatively inexpensive and can be repeated regularly to assess progress with therapy.
The second thing that I recommend is that you gain a working knowledge of your diagnosis. While there are no  perfect sources of information, the internet can provide useful basic information as a starting point. Begin by obtaining from your doctor the most accurate definition of the cancer. If it is breast cancer, is it infiltrating ductal or lobular? Are you ER positive? Is your tumor HER-2 positive? If it is stomach cancer, is it intestinal type or diffuse, etc? This will facilitate your searches, as well as your future conversations with consultants.
perfect sources of information, the internet can provide useful basic information as a starting point. Begin by obtaining from your doctor the most accurate definition of the cancer. If it is breast cancer, is it infiltrating ductal or lobular? Are you ER positive? Is your tumor HER-2 positive? If it is stomach cancer, is it intestinal type or diffuse, etc? This will facilitate your searches, as well as your future conversations with consultants.
Once you know what you’ve got, the next thing you will need to know is where it is. That is what is known as your stage. The older classification used Roman Numerals I-IV with local disease (early) as stage I and metastatic (disseminated) as stage IV. The more modern system is known as TNM, where T stands for tumor size (1-4), N stands for lymph involvement(1-3), and M stands for metastatic involvement (0 or 1). Most contemporary pathology reports include TNM staging. With the diagnosis and stage established, you now know what you have and where it is.
This is where it gets interesting. Now, what do you do about it?
It is at this point that therapeutic choices must be made. Most physicians will rely upon standard established guidelines. Among the most widely used guidelines are those published by the National Comprehensive Cancer Network known as NCCN. While these guidelines can be useful, they can also be stultifying, limiting patients to what might be considered the lowest common denominator of care. While they may be better than haphazard treatment selection, they may very much miss the mark for your unique needs.
Here the process degenerates into a plethora of confusing choices.
Should you have genomic profiling? If so, should it be based on a tissue biopsy, circulating cell free tumor analysis, or even the newer urine tests that measure the presence or absence of abnormal genes? All of these technologies have merit and over the coming years the best ones will shake out. Despite these tests being widely touted (and profitable for the purveyors), none of these test have been put to formal trials that establish their capacity to influence survival. This is interesting because many of these tests have obtained insurance and Medicare coverage without even remotely rising to this standard. Nonetheless, these tests can be used for specific diseases like lung and leukemia where actionable targets are known to exist. Beyond that, caveat emptor (buyer beware).
One of the problems with genomic profiles is that they do very good job of telling you what the problem may be, but a very bad job at telling you the solution. It is a rare genomic mutation that comes with a drug to treat it. Most of the findings wind up asking more questions rather than providing more answers.
With the diagnosis established, the stage known and in certain circumstances molecular profiles complete, it is time for you to choose treatments and the centers that will provide them. Many seek the care of academic centers. These centers may offer clinical trials as a first line therapy for those who meet criteria.
 It should be remembered that clinical trials are conducted in three principal formats. Phase I trials examine brand new drugs. These trials determine the safety of the drugs at different dose schedules. Phase II trials take the established safe doses and develop experience in each type of disease, e.g. lung versus colon versus breast. Phase III trials then compare the new drugs with existing treatments to see if there is any real improvement.
It should be remembered that clinical trials are conducted in three principal formats. Phase I trials examine brand new drugs. These trials determine the safety of the drugs at different dose schedules. Phase II trials take the established safe doses and develop experience in each type of disease, e.g. lung versus colon versus breast. Phase III trials then compare the new drugs with existing treatments to see if there is any real improvement.
It is critical to recognize the functions of these different types of trials. Phase I studies classically have no therapeutic intent (your benefit is secondary to their measurement of your ability to tolerate the drug).
Phase II trials seek evidence of clinical activity by disease, but your specific disease may not be right for that drug.
Finally, Phase III allows a comparison of standard treatment to the new one. Many of these drugs do not make the grade and fall off the development wagon. In addition, you must be willing to be randomly assigned.
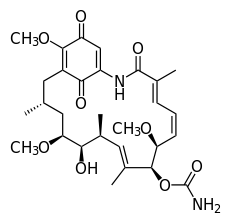
It is here that my approach diverges from those outlined. I have long maintained that each patient is unique and that their cancers must be treated individually. Recognizing that no genomic, proteomic or transcriptomic platform can answer the very complex questions of therapeutic response, we at Rational Therapeutics have developed functional analyses through the use of the EVA-PCA assay, which studies each patient’s tumor by exposing it to the drugs of interest. The most active, least toxic combinations are then recommended. In a report at the American Society of Clinical Oncology meeting of 2013, we showed a 2.02 higher response rate (P < 0.001) and a 1.44 improvement in one year survival (P < 0.02) for patients who received assay-guided therapy. This established the predicative validity of the functional approach.
It is important for patients to realize that cancer is an unbalanced system, not just an abnormal cell. Cancer as a disease goes beyond the cell or even the tumor to affect the body itself. Alterations in immunity, metabolism and physiology contribute to the good or bad outcomes of every patient. Patients should seek to normalize their lifestyle, improve their diets, maintain an active exercise program, reduce their weight to lean body weight, and may in some circumstances consider nutritional supplements and/or appropriately selected natural products that may augment their wellbeing.
The human body is a complicated machine and each part resonates with every other part. A good diet, a good night’s sleep and avoidance of an unhealthy lifestyle, as much as they may sound like your mother’s advice, is indeed very good advice.
Every cancer patient has the right to get better. As a patient, you should take charge of your cancer and make smart decisions. Afterall, no one is more interested in saving your life than you.