In Cancer Research: An Awakening?
February 13, 2015 3 Comments
In 2005, as the Iraq War reached a low point with casualties mounting and public support dwindling, Sunni tribesman in the Anbar Province arose to confront the enemy. Joining together as an ad hoc army these fighters turned the tide of the war and achieved victories in the face of what had appeared at the time, to be overwhelming odds.
I am reminded of this by an article in The Wall Street Journal by Peter Huber and Paul Howard of the Manhattan Institute that examined the bureaucracy of drug development. It raised the question: Are new cancer treatments failures or is the process by which they are approved a failure? They describe “exceptional responders” defined as patients who show unexpected benefits from drug treatments. Using molecular profiles, they opine, scientists will unravel the mysteries of these individuals and usher in an era of personalized medicine. Thus, rigid protocols that use drugs based upon tumor type e.g. lung vs. colon fail because they do not incorporate the features that make each patient unique – an awakening.
The example cited is from Memorial Sloan-Kettering where a patient with bladder cancer had an unexpected response to the drug Everolimus (approved for kidney cancer). Subsequent deep sequencing identified a genetic signature associated with sensitivity to this drug. While it is a nice story, I already knew it very well because it had been repeated many times before and would in the past have been dismissed as an “anecdote.” It is precisely because of its rarity that it has been repeated so many times.
The WSJ analysis strikes a familiar chord. For decades, we have decried the failure of rigid clinical trials that underestimate a patient’s unique biology yet cost millions, even billions of dollars, while denying worthy candidates new treatments under stultifying disease-specific designs.
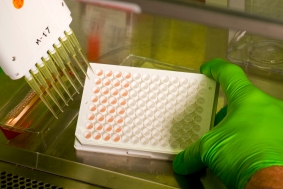 We pioneered phenotypic (functional) analyses (the EVA-PCD platform) to examine whole cell models as we explored drug response profiles, novel combinations and new targets. It is regrettable that these WSJ authors, having raised such important issues, then stumble into the same tantalizing trap of molecular diagnostics, and call for bigger, better, faster genomic analyses.
We pioneered phenotypic (functional) analyses (the EVA-PCD platform) to examine whole cell models as we explored drug response profiles, novel combinations and new targets. It is regrettable that these WSJ authors, having raised such important issues, then stumble into the same tantalizing trap of molecular diagnostics, and call for bigger, better, faster genomic analyses.
Cancer patients need to receive treatments that work. They do not particularly care why or how they work, just that they work. These authors seem to perpetuate the myth that we must first understand why a patient responds before we can treat them. Nothing could be further from the truth.
Alexander Fleming knew little about bacterial cell wall physiology when he discovered penicillin in 1928, and William Withering knew nothing about the role of muscle enzymes in congestive heart failure when he discovered digoxin extracts in 1785. Would anyone argue that we should have waited decades, even centuries to apply manifestly effective therapies to patients because we did not have the “genes sequenced?’
We may be witness to an awakening in cancer drug development. It may be that a new understanding of individualized patient response will someday provide better outcomes, but platforms with the proven capacity to connect patients to available treatments should be promoted and applied today.



Dr. Nagourney,
I would love to use your technology but I don’t have live tumor. When my advanced stage Serous Epithelial Ovarian Cancer recurred in Nov. 2013, I even contacted your office and was advised not to have a second surgery. Therefore, I went through another round of Carboplatin and Taxol. I’m again in remission and wondering what I can do to maintain it. Alas, as I understand it, I cannot use your very effective assay because I don’t have live tumor.
I would love to know what scientifically valid testing I could get to know whether three remission maintenance protocols(off label use of low dose Leukine and Proleukin, Mistletor, Anvirzel – aka oleander – would work. Any suggestions? Thanks.
Faith
It is known that “platinum sensitive” relapses can respond well to re-challenge with Carbo-or Cisplatin based second line therapy. It is gratifying that you have done so well. As to testing the compounds you mention we have examined many natural products. We are very familiar with the oleander extracts as well as iscador (found in mistletoe). Interleukin and other cytokine’s also have activity alone and in combination with other immune augmentative treatments.
However, it can be difficult to predict response to immune therapies due to their dependence upon the interaction between cells like dendritic cells, B-cells, T-cells and macrophages, all of which occur in the microenvironment of the tumor. Small molecules like oleandrengen however can be studied. We continue to examine some these compounds and may in the future have some of the predictive test that you describe.
Thank you for your reply.