Triple Negative Breast Cancer: Worse or Just Different?
March 11, 2014 1 Comment
The term “triple negative breast cancer” (TNBC) is applied to a subtype of breast cancers that do not express the estrogen or progesterone receptors. Nor do they overexpress the HER2 gene. This disease constitutes 15 – 20 percent of all breast cancers and has a predisposition for younger women, particularly those of black and Hispanic origin. This disease may becoming more common; although, this could reflect the greater awareness and recognition of this disease as a distinct biological entity.
On molecular profiling, TNBC has distinct features on heat maps. The usual hormone response elements are deficient, while a number of proliferation markers are upregulated. Not surprisingly, this disease does not respond to the usual forms of therapy like Tamoxifen and the other selective estrogen response modifiers known as SERMs. Nonetheless, TNBC can be quite sensitive to cytotoxic chemotherapy. Indeed, the responsiveness to chemotherapy can provide these patients with complete remissions. Unfortunately, the disease can recur. Complete remission maintained over the first three to five years is associated with a favorable prognosis, with recurrence rates diminishing over time and late recurrences more often seen in estrogen receptor-positive cancers.
Triple negative breast cancer is not one, but many diseases.
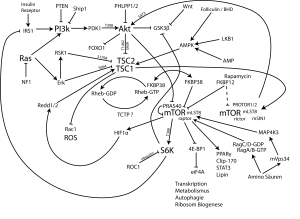 Among the subtypes are those that respond to metabolic inhibitors such as the PI3K and mTOR directed drugs. Another subset may respond to drugs that target epidermal growth factor. There are basal-types that may be somewhat more refractory to therapy, while a subset may have biology related to the BRCA mutants, characterized by DNA repair deficiencies and exquisite sensitivity to Cisplatin-based therapies. Finally, a last group is associated with androgen signaling and may respond to drugs that target the androgen receptor.
Among the subtypes are those that respond to metabolic inhibitors such as the PI3K and mTOR directed drugs. Another subset may respond to drugs that target epidermal growth factor. There are basal-types that may be somewhat more refractory to therapy, while a subset may have biology related to the BRCA mutants, characterized by DNA repair deficiencies and exquisite sensitivity to Cisplatin-based therapies. Finally, a last group is associated with androgen signaling and may respond to drugs that target the androgen receptor.
Some years ago, we used the EVA-PCD platform to study refractory patients with breast cancer and identified exquisite sensitivity to the combination of Cisplatin plus Gemcitabine in this patient group. We published our observations in the Journal of Clinical Oncology and the combination of Cisplatin or Carboplatin plus Gemcitabine has become an established part of the armamentarium in these patients.
The I-SPY-2 trial has now used genomic analyses confirming our observations for the role of platins in TNBC. This i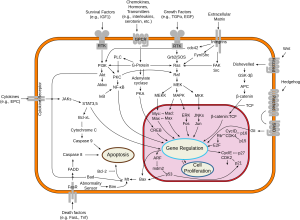 n part reflects the DNA repair deficiency subtype associated with the BRCA-like biology. More recently, we have examined TNBC patients for their sensitivity to novel therapeutic interventions. Among them, the PI3K and mTOR inhibitors, as well as the glucose metabolism pathway inhibitors like Metformin. Additional classes of drugs that are revealing activity are the cyclin-dependent kinase inhibitors, some of which are moving forward through clinical trials.
n part reflects the DNA repair deficiency subtype associated with the BRCA-like biology. More recently, we have examined TNBC patients for their sensitivity to novel therapeutic interventions. Among them, the PI3K and mTOR inhibitors, as well as the glucose metabolism pathway inhibitors like Metformin. Additional classes of drugs that are revealing activity are the cyclin-dependent kinase inhibitors, some of which are moving forward through clinical trials.
One feature of triple negative breast cancer is avid uptake on PET scan. This reflects, in part, the proliferation rate of these tumors, but may also reflect metabolic changes associated with altered glucose metabolism. In this regard, the use of drugs that change mitochondrial function may be particularly active. Metformin, a member of the biguanide family influences mitochondrial metabolism at the level of AMP kinase. The activity of Metformin and related classes of drugs in triple negative breast cancer is a fertile area of investigation that we and others are pursuing.
When we examine the good response of many triple negative breast cancers to appropriately selected therapies, the potential for durable complete remissions and the distinctly different biology that TNBC represents, the question arises whether TNBC is actually a worse diagnosis, or simply a different entity that requires different thinking. We have been very impressed by the good outcome of some of our triple negative breast cancer patients and believe this a very fertile area for additional investigation



I would like to thank Dr Nagourney for his important work. Because of the profound failure of the conventional war on cancer, prevention should be the focus with diet, nutrition, exercise, stress reduction, sleep. Epigenitics is the future. Chemotherapy, radiation, surgery and genetics are so yesterday. Glucose metabolism pathways are one of the important “new directions in the war on cancer.”